Current methods of anticoagulation monitoring: Heparin is usually monitored with the APTT (activated partial thromboplastin time) method. It tests the time it takes for your blood to clot [14].
Problems with method: Can’t always accurately predict things. Current methods are the best we have, but technology is not good enough yet [15].
Other methods, such as activated clotting time (ACT) and anti-factor XA are used, though they are not as accurate, or do not provide enough information [15].
A balance is needed to prevent bleeding and clotting. Anticoagulation tests are needed to determine how much anticoagulant to use, however, these tests are not always accurate. Current methods are limited and not good enough [14].
Test results vary among individual, and test procedure varies among ECMO centers. The standard range of test results may not accurately predict the clotting time for different individuals [13],[16].
Our criteria:
- Accurate blood clot formation time prediction.
- Does not interfere with body activities.
- Detect blood clots through their chemical or physical property [13].
- Affordable.
- Constant monitoring.
- Compatible Biomaterial for the Tubing used in the ECMO machine
| Accurate prediction of
coagulation time Accurate prediction of coagulation time |
|
| Safety |
|
| Biomaterial of the tube to prevent coagulation of blood within tubes
Biomaterial of the tube to prevent coagulation of blood within tubes |
|
| Constant Monitoring |
|
| Limitations
Limitations |
|
| Cost |
|
| Contraindication |
|
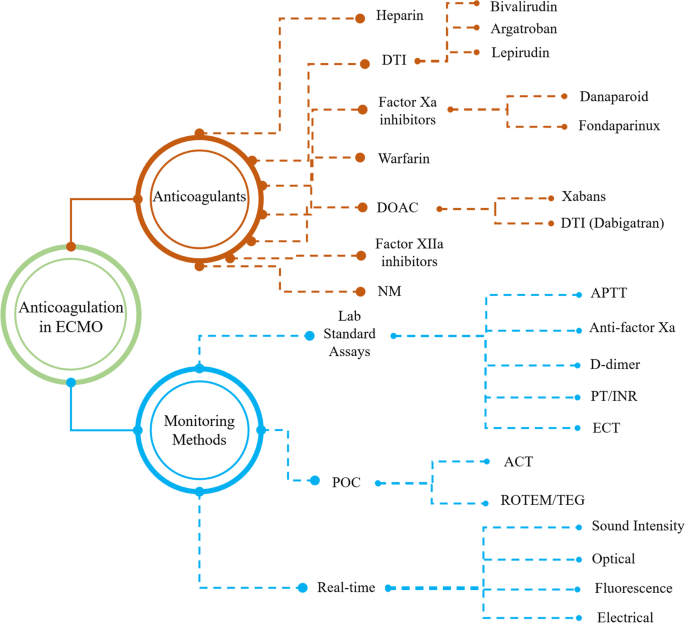
Various anticoagulants used in ECMO devices and their monitoring methods[13].
References
- [11]Zeibi Shirejini, Saeedreza, et al. “Current and future strategies to monitor and manage coagulation in ECMO patients.” Thrombosis Journal, vol. 21, no. 1, 2023, https://doi.org/10.1186/s12959-023-00452-z.
- [12]Kumar G, Maskey A. Anticoagulation in ECMO patients: an overview. Indian J Thorac Cardiovasc Surg. 2021 Apr;37(Suppl 2):241-247. doi: 10.1007/s12055-021-01176-3. Epub 2021 Mar 23. PMID: 33967447; PMCID: PMC8062644.
- [13]Chlebowski, M.M., Baltagi, S., Carlson, M. et al. Clinical controversies in anticoagulation monitoring and antithrombin supplementation for ECMO. Crit Care 24, 19 (2020). https://doi.org/10.1186/s13054-020-2726-9
- [14]Tung Phi Nguyen, Xuan Thi Phan, Dai Quang Huynh, Ha Thi Viet Truong, Yen Nguyen Hai Le, Tuan Manh Nguyen, Quan Quoc Minh Du, Thao Phuong Le, Hai Ngoc Truong, Thi Thi Ho, Thao Thi Ngoc Pham, “Monitoring Unfractionated Heparin in Adult Patients Undergoing Extracorporeal Membrane Oxygenation (ECMO): ACT, APTT, or ANTI-XA?”, Critical Care Research and Practice, vol. 2021, Article ID 5579936, 7 pages, 2021. https://doi.org/10.1155/2021/5579936
- [15]Lee, S., Chaturvedi, A. Imaging adults on extracorporeal membrane oxygenation (ECMO). Insights Imaging 5, 731–742 (2014). https://doi.org/10.1007/s13244-014-0357-x
- [16]https://www.hopkinsmedicine.org/health/conditions-and-diseases/coagulation-disorders#:~:text=Coagulations%20disorders%20are%20conditions%20that,thrombosis%20are%20all%20coagulations%20disorders
- [17] https://www.testing.com/tests/partial-thromboplastin-time-ptt-aptt/